
FEATURE – Are you getting tested too much? Not often enough? For the right things? More testing is generally better, right? This will catch you up on what you need to know about this important subject.
The following 10 items are based on recommendations from the National Institute of Health. Things have changed some in the last few years. See if you are up to date:
1 – Hypertension.
Screening for hypertension should begin at age 18 and, if there are no other risk factors, checked every three years until age 40 then yearly. You can do it yourself. If one random blood pressure is high, take it again several times over the next month or two.
Data from recent large studies shows benefits to pushing blood pressure lower than we used to. The newer goal in women with risks of heart attack and stroke is 120/70. This lower goal is a fairly recent change and comes from a huge trial published in the New England Journal of Medicine in what is called the Sprint trial.
2 – Cholesterol levels (lipids) to prevent heart disease.
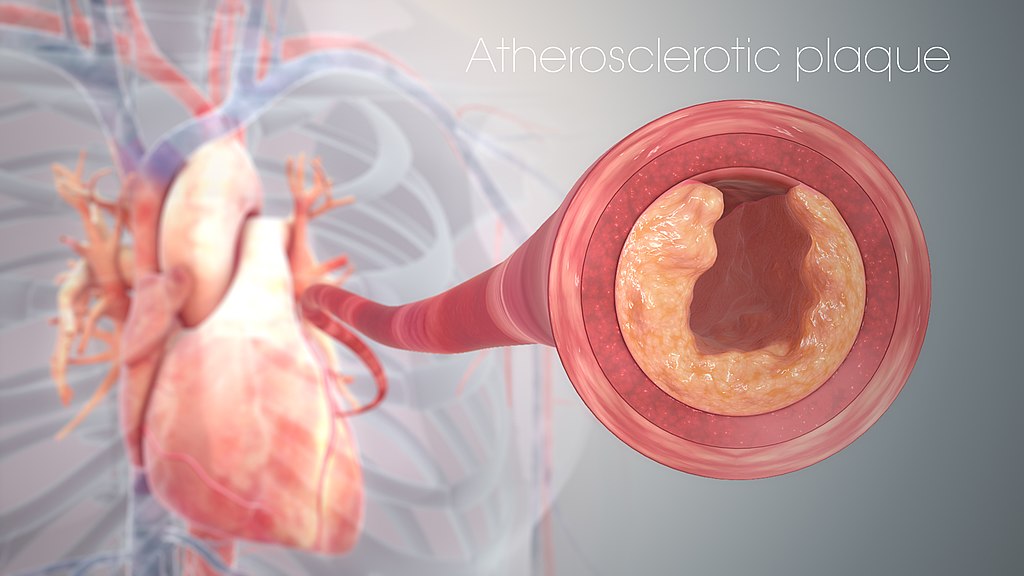
Screening for high cholesterol should start about age 45 and if normal every five years is reasonable. These tests are typically being done on women too early and too often. Studies show that low-risk women do not benefit from taking cholesterol-lowering medications unless their 10-year risk of a heart attack or stroke is over 7.5 percent.
Women and men are different when it comes to heart disease, too. They have different risks and often have different symptoms. More frequent testing and more aggressive treatment of elevated lipids in low-risk patients do not reduce mortality from heart attack.
3 – Diabetes.
Screening for diabetes at 40 is recommended then every three years if there are risk factors. If there are no significant risk factors, you do not need to be tested any more frequently than every five years.
4 – Colon cancer.
Screening for colon cancer with colonoscopy every 10 years starting at age 50 is the best screening test for colon cancer, which is the second most common cancer in nonsmoking women. Colonoscopy decreases mortality from colon cancer by over 75 percent. It is quick and safe, and appointments can usually be made by calling a gastroenterologist directly for routine screening.

5 – Cervical cancer.
Screening for cervical cancer (Pap smears) should not start before age 21 and if it is normal then every three years.
Screening is slowly moving away from Pap smears and towards screening for high-risk HPV (human papilloma virus) instead because it is this virus that causes cervical cancer. An effective HPV vaccine is available now and screening decreases mortality by over 75 percent. Paps are usually discontinued at age 65.
6 – Ovarian cancer.
Screening for ovarian cancer is not recommended in average-risk women. Hopefully that will change in the near future, but presently there are no effective screening methods for a low-risk population. CA-125 blood tests are used to follow known ovarian cancers and their response to treatment, but it is not an effective screening tool.
7 – Lung cancer.
Screening for lung cancer is recommended yearly for moderate to heavy smokers over 55 by performing low-dose CT scanning (formerly known as a CAT scan). Screening reduces death from lung cancer by 20 percent. Lung cancer is the No. 1 cause of cancer death in women and has the highest five-year mortality rate of any cancer. Women who smoke are 13 times more likely to get lung cancer than those who don’t.

8 – Breast cancer.
Screening for breast cancer with mammography is recommended to start at age 40-50 at one- to two-year intervals (there is no consensus). The reason there is no consensus is that mammograms unfortunately show only a very small decrease in breast cancer mortality, and self-exams are no longer encouraged because of lack of evidence.
Look for an upcoming feature in which I will talk about what mammography does and doesn’t do for you in greater detail. It is very important for women to have a clear idea of what the risks and benefits are of mammography to make informed decisions about their health. Coming soon ….
9 – Skin cancer.
Depending on your risks, it is recommended to have a skin exam every one to three years if you have risk factors for melanoma as recommended by your dermatologist. If you are at low risk, your primary doctor (family practitioner or OBGYN) should be able to screen your skin for skin cancers and pre-cancerous changes.
Of the three main types of cancers (basal cell, squamous cell and melanoma), only melanomas are metastatic and potentially fatal. They can be anywhere (even in places that the sun doesn’t shine). Make sure your skin gets carefully examined.
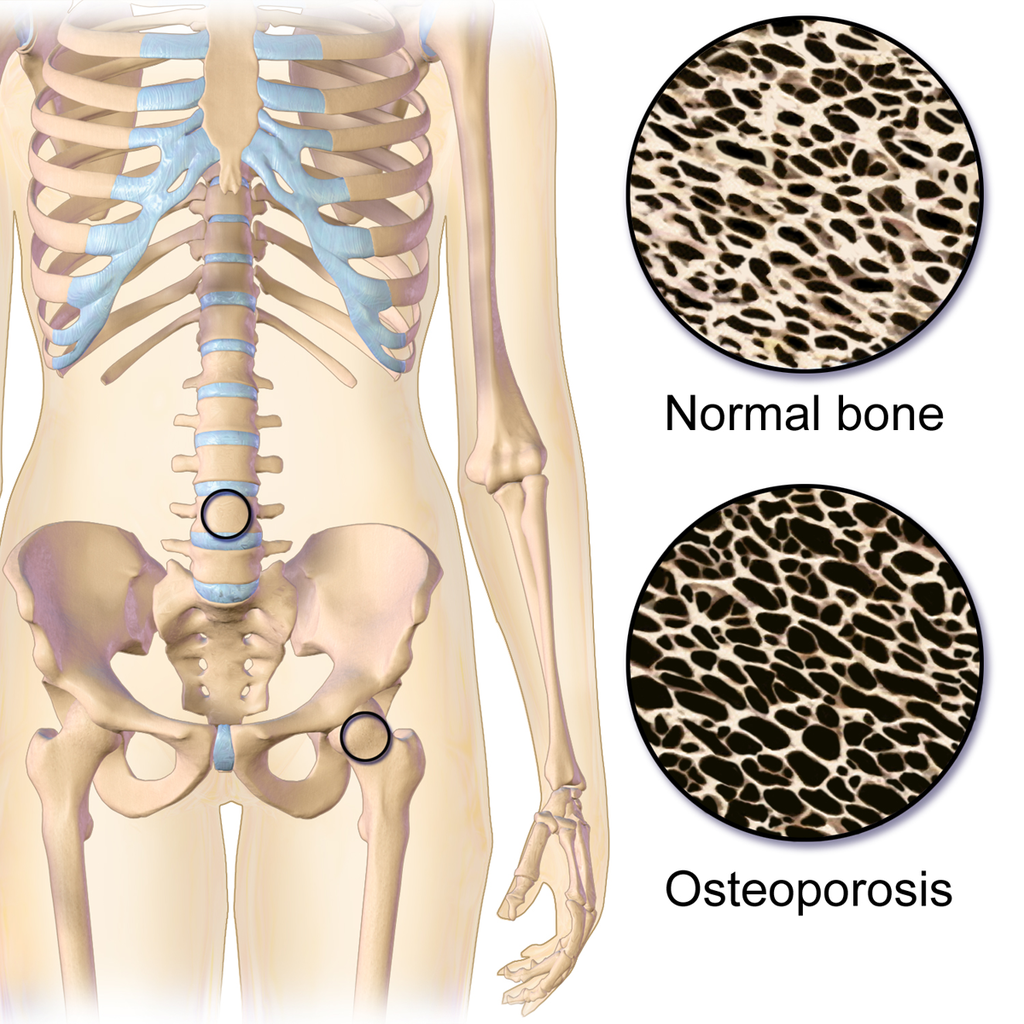
10 – Osteoporosis.
Screening for osteoporosis in normal-risk women should not start until age 65 or about 15 years after entering menopause. Screening is done by DEXA scan (like an X-ray). If your bone density is normal, current recommendations are that you do not need to be tested again for 10-15 years.
If your DEXA/fracture risk shows some thinning of bone (osteopenia), you should be tested no sooner than every three years. Data shows that more frequent or earlier testing is not effective.
One final suggestion: All other screening, lab work and testing should be based on specific concerns or risks.
- Many people get thyroid tests, blood counts, liver function testing and renal testing just as routine. These are not recommended screening tests.
- Getting blood work just out of routine every year is not recommended, is unnecessarily expensive (increasing the costs of health care even more) and is not beneficial to you.
Knowledge is power. You have every right to participate in the decisions regarding how you are screened and treated for disease. Like everything else in life, the more you know, the better you can be involved with your own health care.
Resources
- Dr. Sean Lynn practices at St. George Women’s Health Center, St. George | Telephone: 435-218-7770.
Email: [email protected]
Twitter: @STGnews
Copyright St. George News, SaintGeorgeUtah.com LLC, 2018, all rights reserved.